%20(1).jpg)
Subutex and Suboxone are two medications commonly prescribed to patients struggling to overcome an opioid dependence. Both treatment options are approved by the U.S Food and Drug Administration (FDA) for the treatment of opioid use disorder (OUD).
The main difference between Subutex and Suboxone is that the former does not contain naloxone, which was initially thought to raise the risk of miscarriage or adverse fetal outcomes. However, research suggests that Suboxone, which does contain naloxone, is as safe and efficacious as Subutex.
When Medication for Addiction Treatment (MAT) first became available for pregnant women with OUD, Methadone was the standard of care. However, in the U.S., Methadone must be administered at a licensed opioid treatment program. This created and continues to create barriers to receiving MAT for patients who cannot make daily visits to a methadone program.
In later years, pharmacotherapy with buprenorphine became recognized as comparable in efficacy and safety to methadone, with the advantage that it can be obtained at a doctor’s office and does not require daily attendance at a methadone program. [1]
Both methadone and Suboxone can be used during pregnancy. Neither is necessarily “superior” during pregnancy, however Suboxone does have some advantages in pregnancy:
First, research shows that Suboxone often results in less severe Neonatal Abstinence Syndrome compared to methadone.[2]
Second, Suboxone is also considered safer than methadone in terms of overdose risk.[3].
The two most well-known buprenorphine formulations used in pregnancy are Subutex (the brand name for buprenorphine-monotherapy) and Suboxone (the brand name for buprenorphine combined with naloxone).
Buprenorphine is safe for pregnant and breastfeeding women. Buprenorphine is listed as a Category C medication, meaning there is little data on its effects in certain human populations, but is generally considered safe in pregnancy.[1] MAT, including Suboxone, is recommended for all pregnant individuals who struggle with opioid use disorder (OUD). The American College of Obstetrics and Gynecology (ACOG) announced in 2017 their support for use of buprenorphine/naloxone during pregnancy. [8]
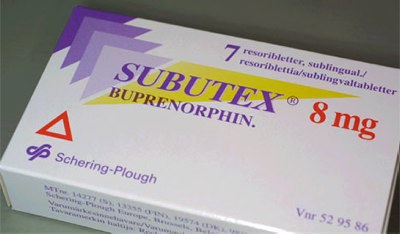
Subutex is the commonly known brand name for buprenorphine monotherapy. It is a safe and effective medication used to treat OUD. Subutex is similar to Suboxone but does not contain Naloxone. It was originally designed as a formulation for pregnant women because it was not known whether or not naloxone was teratogenic (having potential harms to a developing fetus). Subutex, just like Suboxone, is administered sublingually (via films under the tongue).
Suboxone is a brand name medication commonly prescribed by clinicians to treat OUD, and it is a combination of two medications: buprenorphine and naloxone. Buprenorphine is a partial opioid that suppresses cravings and naloxone (commonly known as Narcan) is an opioid antagonist that blocks opioids in the brain, added to buprenorphine in order to prevent overdose in case the medication is injected inappropriately.
Initially, pregnant women were prescribed Subutex instead of Suboxone because it was unknown whether the naloxone component of Suboxone might be dangerous to a developing fetus. Now, however, more research has been done on Naloxone in pregnancy, and it is generally thought to be safe. Research from the American College of Obstetrics and Gynecology (ACOG) in 2017 confirmed that outcomes were similar between women on buprenorphine-naloxone when compared with women on buprenorphine alone, with no increased risk of adverse events. [8] Now, pregnant women can either start Subutex or simply continue Suboxone if they were on it prior to pregnancy.
The only difference between Suboxone and Subutex is the presence of naloxone. When taken appropriately under the tongue, the Naloxone in Suboxone is not absorbed and does not produce many significant side effects [6] Most of the side effects experienced from taking either Subutex or Suboxone are associated with buprenorphine, not naloxone. Thus, the side effects of Suboxone and Subutex are extremely similar.
It is possible to have a sensitivity or allergic reaction to naloxone, but this is very rare. If you are concerned about this possibility or have had an allergic reaction to naloxone before, Suboxone may not be a good option. Talk to your doctor as you might be better suited to a medication like Subutex.
Pregnant women tend to experience the same side effects with Suboxone as non-pregnant women. The most common of these include dizziness, sedation, or nausea. These symptoms tend to abate as the body gets accustomed to the medication.
If you cannot manage side effects on your own, your doctor can either adjust your dose or offer options to manage common side effects. This might include the following:
More serious side effects like palpitations, fever, or respiratory distress should be immediately reported to your doctor so you can receive medical attention.
The main side effect of both Subutex and Suboxone is Neonatal Abstinence Syndrome (NAS). NAS refers to the non-life threatening withdrawal symptoms experienced by newborns whose mothers are on Suboxone or Subutex during pregnancy.
Signs of NAS occur within 72 hours after birth and include the following symptoms:
Any of the recommended OUD treatments, including methadone and buprenorphine — as well as other substances such as nicotine, selective serotonin reuptake inhibitors, and benzodiazepines — may bring on NAS. NAS occurs in 30–80% of infants born to women taking opioid agonist therapies.
Suboxone and Subutex both carry risk of neonatal abstinence syndrome. However, the good news is that both Suboxone and Subutex cause a milder form of neonatal abstinence syndrome than other full agonist opioids such as Methadone, heroin, or other prescription pills. Taking a buprenorphine-based medication during pregnancy was shown in a 2012 study to reduce neonatal distress compared to full opioid agonists. Full opioids are associated with low birth weight, preterm birth, and a higher risk of infant mortality.[2] Taking Suboxone instead of full opioids can mitigate these risks.
Most providers in the United States agree that the benefits of Buprenorphine therapy greatly outweigh the risks and generally recommend buprenorphine therapy for pregnant women with OUD. As to whether Subutex or Suboxone is “better”, the answer is not clear. It certainly seems that both are equally safe in pregnancy. Subutex was historically given because it did not contain Naloxone, however this risk has been largely debunked in more recent years. [8]. Most providers do not routinely transition women on Suboxone to Subutex during pregnancy, given that “transferring a pregnant patient to a different opioid agonist that has greater abuse potential might not be necessary.”[10]
One slight advantage to Suboxone is that the Naloxone component prevents the medication from getting a patient “high” if they were to inject it, reducing the risk of overdose, including in pregnant women [5]. On the other hand, Subutex is less commonly prescribed and might be slightly more logistically difficult to obtain. It may also not be paid for by certain insurances.
Overall, both medications are equally effective in pregnancy. Talk to your doctor about which might be the most feasible and effective medication for you to use during pregnancy.
After giving birth, switching from Subutex to Suboxone is not only feasible, but often preferred to reduce the diversion/misuse risk associated with Subutex, which can be more easily injected and misused. Some insurance plans may not cover Subutex outside of pregnancy, and thus it might be necessary to switch to Suboxone for coverage reasons, depending on your insurance. You can help determine what forms of buprenorphine will be covered by your insurance plan by calling your plan directly.
Leading medical organizations such as ACOG, SAMHSA and CDC all have concluded that breastfeeding is generally beneficial in women taking methadone or buprenorphine medications, unless they have contraindications, such as HIV infection, or are using other illicit drugs.
Not only does breastfeeding contribute to attachment between a woman and her infant and facilitates skin-to-skin care, it also provides immunity to the infant. It has been shown to reduce symptoms of neonatal abstinence syndrome as well.
Furthermore, the American Academy of Pediatrics recommends breastfeeding for women taking methadone and buprenorphine regardless of maternal dose, because transfer of these medications into breast milk is minimal.[10]
Untreated OUD in pregnancy is dangerous, and guidelines encourage all pregnant mothers to take MAT.
If you have questions about whether Medication for Addiction Treatment (MAT) is a fit for you, schedule a time to speak with one of our MAT professionals, or call us today at (844) 943-2514.
Subutex image by ZngZng under a Creative Commons Attribution 2.0 Generic license.
Bicycle Health provides Suboxone therapy for opioid use disorder. Bicycle offers educational resources on Belbuca, Subutex and Sublocade, but does not currently offer those therapies.
%20(1).jpg)
Elena Hill, MD; MPH received her MD and Masters of Public Health degrees at Tufts Medical School and completed her family medicine residency at Boston Medical Center. She is currently an attending physician at Bronxcare Health Systems in the Bronx, NY where she works as a primary care physician as well as part time in pain management and integrated health. Her clinical interests include underserved health care, chronic pain and integrated/alternative health.
Our science-backed approach boasts 95% of patients reporting no withdrawal symptoms at 7 days. We can help you achieve easier days and a happier future.
Get Startedor book an enrollment call